Mechanical Low Back Pain:
- Mechanical Low Back Pain, also known as non-specific back pain, is the general term used for any type of pain that is arising from abnormal stress and strain on the muscles and joints of the vertebral column and is one of the most common musculoskeletal complaints
- Can be secondary to many factors, including: trauma, disc herniation, spinal stenosis, lumbar sprain or strain, spondylolysis, spondylolisthesis and scoliosis.
- Often associated with non-biological factors
- Can be both acute and chronic in nature; chronic pain is persistent pain of more than 3 months following injury or surgery where the true source is difficult to determine
Subjective Examination:
Can be traumatic or non-traumatic
Can be in a specific area or globalised pain around the lumbo-sacral region and can refer into the buttocks, tops of the legs and thighs
Usually aggravated by prolonged static load of the spine, poor posture, lifting heavy objects, levered postures, road traffic collisions
May be associated with morning stiffness of less than a 30 minute duration
Objective Examination:
Altered gait pattern
Altered or poor posture
Absence of neurological signs
Can have reduced range of movement but not in all cases
Often associated with increased paraspinal musculature activation but again not in all cases
Early signs to look out for:
Red flags for lower back pain that include: cancer, unexplained weight loss, unremitting night pain, immunosuppression, prolonged use of steroids, intravenous drug use, urinary tract infection, fever, significant trauma, bladder/ bowel incontinence, urinary retention and saddle anesthesia
Rule out additional causes that include infection, neoplasia, metabolic disease, inflammatory rheumatological disorders and referred pain
Additional non-biological factors
References
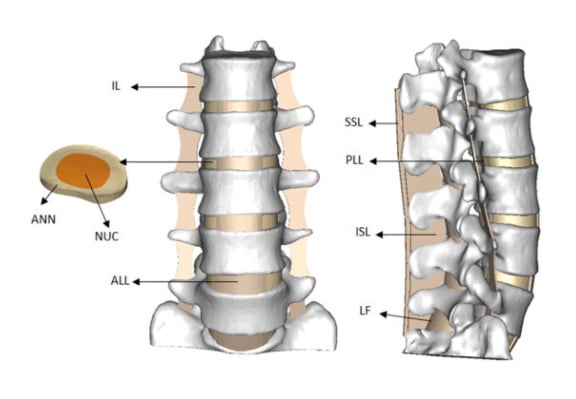
Image from OpenI – Licensed by CC
Image from OpenI – Licensed by CC
Treatment:
Rule out any serious underlying pathology and non mechanical causes
Strong encouragement of self management and return to normal activities, as tolerated, to lead to a more rapid recovery
Adequate analgesia
Refer to Physiotherapy to commence an exercise program to prevent debilitation. The Physiotherapist can work with the patient on lifestyle strategies to help with long term management.
References
Image from OpenI – Licensed by CC
Image from OpenI – Licensed by CC