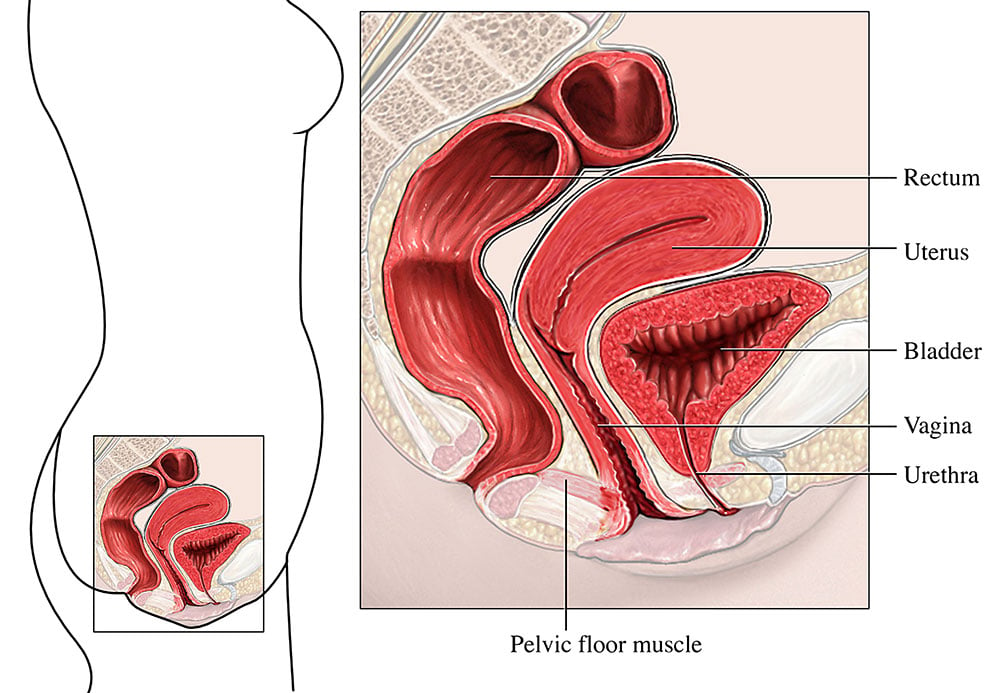
Pelvic organ prolapse:
- Pelvic organ prolapse (POP) is the descent of one or more of the anterior vaginal wall, posterior vaginal wall, the uterus (cervix), or the apex of the vagina (vaginal vault or cuff scar after hysterectomy).
- Presence of any pelvic organ prolapse sign should be correlated with relevant POP symptoms.
- Risk factors include increasing age, parity and family history along with obesity, heavy lifting and constipation.
- A common problem, occurring in up to 40% of women older than 50 years, which may impact on daily activity and quality of life.
Main presenting features:
- Symptoms vary depending on the site and severity of the prolapse. The symptoms are likely to vary over the course of the day and over a period of time, including through the monthly cycle in pre-menopausal women.
- A patient with prolapse might present with vaginal, bladder, bowel, back, abdominal and sexual symptoms, including feeling of ‘something coming down’, pelvic pressure (heaviness, dragging), incomplete bladder or bowel emptying (possibly with the need to support the vaginal wall to aid emptying), low back ache, pain or difficulty during sexual intercourse and vaginal bleeding, discharge or infection.
- Pelvic organ prolapse may be so severe that there is protrusion of the vaginal wall and/or cervix/vaginal vault below the vaginal introitus.
- Symptoms are likely to be increased by gravity (e.g. standing for prolonged periods) and abdominal straining (e.g. after a period of heavy work/lifting).
Your assessment before referral:
Perform a vaginal examination to identify presence of pelvic organ prolapse or pelvic mass. If no prolapse is detected it may be useful to repeat the examination with the woman in a standing position or to ask her to book another appointment to repeat the examination at a different time (the end of the day and/or when she knows her symptoms are likely to be worse).
All patients presenting with associated urinary incontinence/symptoms should undertake a urine dipstick screening to detect the presence of blood, glucose, protein, leucocytes and nitrites in the urine.
Physiotherapy management:
If you feel that your patient has mild to moderate pelvic organ prolapse refer her to physiotherapy. The physiotherapist will complete a detailed assessment, following which she will work with your patient, with the aim of resolving or reducing her symptoms. This may include:
Advice on an individualised pelvic floor muscle exercise programme.
Education on daily activities, general exercise, lifting, diet, weight loss and avoidance of constipation.
Advice on how to achieve optimal bladder and bowel emptying.
If urinary symptoms are present these will be treated accordingly
If conservative management fails the physiotherapist may discuss referral to the gynaecological consultant.
Referrals to consultant-led services:
If your patient describes any of the following symptoms she should be referred directly to the appropriate consultant-led service (following locally-agreed pathways):
Symptomatic prolapse at or below the introitus
Post-menopausal vaginal bleeding
Post-coital bleeding
Persistent intermenstrual bleeding
Unexplained abdominal, bowel or urinary symptoms
Vulval lump, bleeding and/or ulceration
Palpable abdominal/pelvic mass