Frozen Shoulder
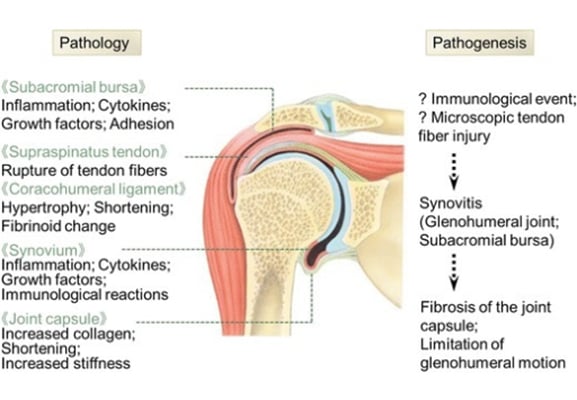
Adhesive capsulitis (frozen shoulder):
- Common condition affecting 3 – 5% of the general population and 20% of the diabetic population.
- Often described as self-limiting; the majority of which resolve in 1-3 years although some patients will experience longer term movement deficit which lasts up to 10 years.
- A typical patient would be female in her 5th to 7th decade of life
- Rarely occurs simultaneously bilaterally although it can occur sequentially bilaterally.
- Normally classified as either primary: insidious onset of pain and progressive loss of movement at the shoulder or secondary; generally due to some form of trauma or subsequent immobilisation.
There are three distinct clinical phases:
- Freezing/painful stage; pain, worse at night decrease active and passive movement. Generally lasts for 3 – 9 months and is characterized by an acute synovitis of the glenohumeral joint
- The frozen/transitional stage. There is little change to the level of pain during this stage but range of movement loss can progress further. Lasts 4 – 12 months. A capsular pattern is therefore evident with most loss of external rotation followed by flexion/abduction and then internal rotation
- Thawing stage; starts when range of movement at the joint begins to improve. Generally lasts 12 – 42 months
Subjective History:
The patient will present with insidious onset of shoulder and upper arm pain which may progress down the arm coupled with gradually reducing range of movement.
Occasionally the patient may present with the onset of the above symptoms following trauma
Pain is often worse at night time.
Objective Examination:
On examination there will be a marked reduction in passive range of movement of the shoulder joint in a capsular pattern with most loss of external rotation followed by flexion/abduction and then internal rotation
Passive abduction of the shoulder will produce early scapular rotation ( typically below 80 degrees abduction)
Radiograph will be clear and help rule out differential diagnosis of pathologies which would produce a capsular pattern at the shoulder such as osteoarthritis.
References
Image from OpenI – Licensed by CC