Spinal Stenosis:
“Stenosis has been found in 80% of subjects over 70 years” (Szpalski & Gunzburg, 2003.) Normal intervertebral height is 20-23mm. If this height is reduced to <15mm then spinal stenosis is likely (Janis & An, 2000.) An extended position (such as standing or walking) is thought to reduce intervertebral space by 15%, therefore making symptoms worse. A flexed position (such as sitting) is thought to increase the space by 12%, therefore reducing pressure on the nerve and relieving symptoms (Janis & An, 2000.)
Differential diagnosis:
Arterial Claudication.
Nerve root irritation from disc prolapse/herniation.
Non-specific mechanical LBP, with somatic referred pain.
Subjective Assessment
The main symptoms associated with stenosis are: leg pain; weakness in the legs; limited walking/standing; numbness or P&N in the legs (either unilateral or bilateral symptoms.)
Does it progressively worsen with walking or other extended positions, such as standing?
Does it ease with flexion, such as sitting or walking with a trolley? (note- Easing symptoms in flexion would also help to differentiate between a neurological claudication or a arterial claudication.)
Clear red flags.
Objective Assessment
Assess ROM of the lumbar spine- ruling out referred symptoms from other lower limb joints.
Neuro assessment (SLR; PKB; Myotomes; Reflexes; Dermatomes- note may or may not have signs of Nerve Root Irritation (NRI) depending on specific changes.
You could try the patient on a static bicycle- this is a flexed position, and if the leg pain was neuropathic claudication then the leg symptoms would not be present, however if arterial claudication then cycling would still bring on the symptoms.
Assess pedal pulses
Further investigations:
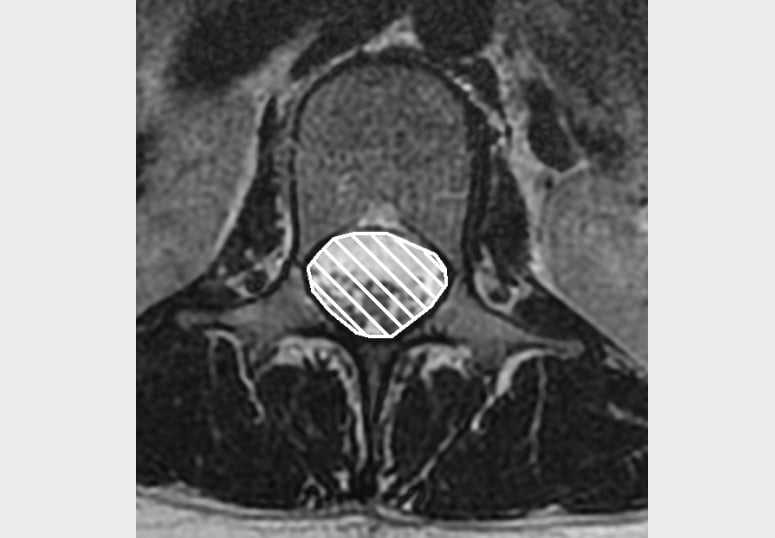
MRI Scan- can be used to view the nerve as it leaves the foramen, and assess any compromise or compression on the nerve. This can be organised BANS.
References
Image from OpenI – Licensed by CC
Image from OpenI – Licensed by CC
Treatment
First line management:
To consider anti-neuropathic medication if appropriate
For patients with Central Canal stenosis physiotherapy would be the management choice initially.
Patients who do not appear to have central canal stenosis, but who have non-resolving sciatica for > 6/52, can be referred to BANS.
Stretch lumbar spine to regain full (normal) ROM. Most likely restriction will be extension, therefore stretch into extension. +/- joint mobilizations as able/tolerated.
General conditioning work, to increase fitness and perhaps improve vascularisation around the spine. May tolerate static cycle (as in a flexed and therefore more ‘open’ position.) Try and increase pain free walking distance (by pacing well, and taking regular breaks to sit/flex.)
Pacing advice, and advice on activity modification. This is twofold, will either allow the patient to “self-manage” their symptoms, or will help to reduce aggravation and symptoms may settle.
References
Image from OpenI – Licensed by CC
Image from OpenI – Licensed by CC